Meet Your ‘Digital Twin.’ They Might Save Your Life.
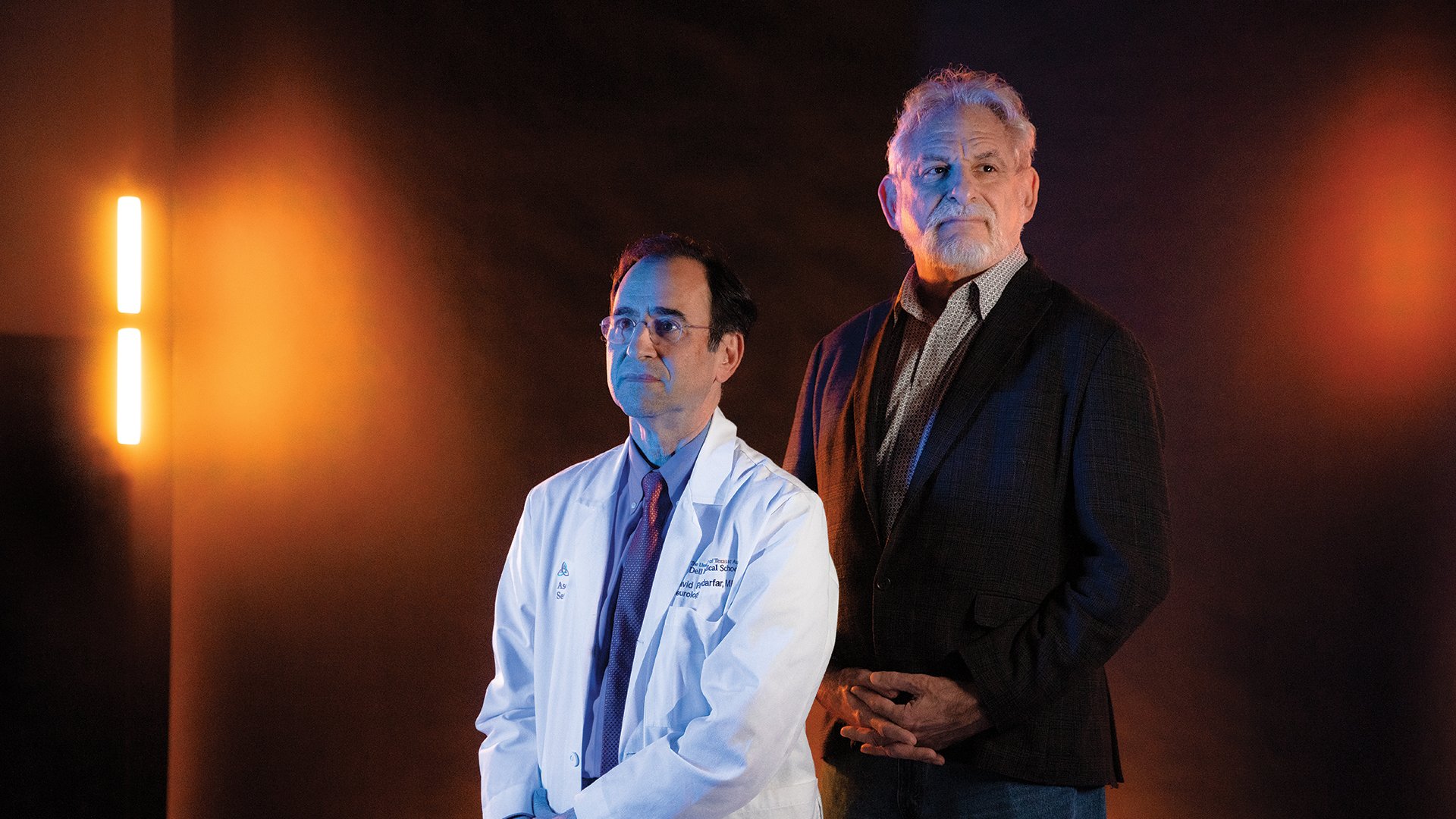
David Paydarfar, M.D., & Michael Sacks, Ph.D.
With advanced computational modeling that uses clinical data collected directly from the patient, “digital twins” will be able to pinpoint exactly how — and when — to treat neurovascular disease.
UT Partnerships
- Cockrell School of Engineering
- Dell Medical School
- The Oden Institute for Computational Engineering and Sciences
External Partnerships
- UCLA
- University of Washington
A person can live for years with an aneurysm (a bulging in a blood vessel), never knowing if — or when — it will fatally rupture. But by using patient data to construct what’s known as a “digital twin,” clinician-scientists will be able to predict not only when a person’s aneurysm may burst, but how they’ll respond to treatment.
It’s the focus of David Paydarfar, M.D., chair of Dell Med’s Department of Neurology and director of the Mulva Clinic for the Neurosciences, and Michael Sacks, Ph.D., professor in the Department of Biomedical Engineering at UT’s Cockrell School of Engineering. Much like hurricane forecasting technology relies on thousands of observed hurricanes, Paydarfar and Sacks’ team is working to build a massive database of patient data to accurately model future outcomes.
“This builds on the idea that no two people are identical,” Paydarfar says. “Let’s take a patient we’ll call Mr. Smith: So you have his age, his gender, sex, risk factors, blood pressure and so forth; all that demographic and medical data has to be paired with this computational tour de force to determine the chance that Mr. Smith will have this rupture in the next day, in the next week, in the next month, in the next year — or at all.”
From Abstract Models to Personalized Medicine
Until now, standard modeling techniques have relied on theoretical data rather than real clinical data taken from the individual patient in question.
“So what's the difference between a digital twin model and a conventional model? It really boils down to the ability to make it ‘updatable’ and be able to utilize it in the hospital or clinic,” says Sacks, who directs the James T. Willerson Center for Cardiovascular Modeling and Simulation at the Oden Institute for Computational Engineering and Sciences. “Being able to use additional data that becomes available — imaging or physiological or genetic data, for example — to update and improve the model is key.”
A critical part of Paydarfar and Sacks’ work to this point has involved bringing in experts in MRI technology to produce crystal-clear, 3D “movies” of the blood vessels pulsating with each heartbeat. They provide the needed detail for accurate forecasting.
“UT really has the potential to be a unique site for these kinds of breakthroughs,” Paydarfar says. “In a project and team like this, you have an interventional vascular neurologist, a computational neurologist, a clinician and computational physicist, and an applied biomedical engineer all collaborating. That sort of team is very hard to replicate. We just have an enormous opportunity here with that depth and breadth of knowledge.”
